When I competed dental school in 2013, MTA was a topic of discussion in the endodontic department. However, as students we were told it was too expensive, too hard to handle, and turned teeth black. Just a few years later, the market has been flooded with new bioceramics that are less expensive, easier to handle, and don’t stain. While this is great news, I wasn’t taught how to use MTA in dental school, and some of the things I was taught we’re finding out are not true. Fortunately, I’ve been able to further my education and have learned to work with these materials to achieve more favorable clinical outcomes.
As a practitioner, my goal is to provide the best care possible to my patients, and that means keeping vital teeth alive. Reaching this goal helps me achieve three things: 1) improve access to care for underserved children (patients with state-funded insurance are less likely to have the opportunity to see an endodontist), 2) prolong tooth life, and 3) avoid the cost of more expensive and time-consuming procedures such as non-surgical root canal therapy.
Patients presenting with dental trauma or deep carious lesions in permanent teeth can greatly benefit from the use of bioceramics. The goals of treatment for these teeth should be to maintain a vital, healthy pulp, and conserve tooth structure. The development of bioceramics has provided practitioners treatment options based on sound evidence, and allows them to utilize more conservative treatment modalities to treat these carious or damaged teeth.
Dental Trauma
A common use for bioceramics in treating dental trauma involves dealing with a complicated fracture or a fracture where the pulp is exposed. In such cases, a partial pulpotomy can be performed to preserve pulp vitality. Using bioceramics can be extremely advantageous in cases where the apex of the tooth has not closed, allowing apexogensis to occur. Complicated fractures or fractures that expose the pulp may be accompanied by other dental injuries such as luxation, but can still be treated with a partial pulpotomy. A partial or Cvek pulpotomy is a procedure that removes a portion of the coronal pulp to help maintain vitality of the radicular pulp. Success rates have been reported to be 81–96 percent. The procedure can be performed days after the trauma occurred, if healthy radicular pulp is apparent (see Figure 1).
Understanding Caries Progression
It is well established scientifically that dental caries is caused by the presence of a biofilm on tooth structure fueled by a substrate. The most commonly associated bacteria are Streptococcus mutans, Streptococcus sobrinus, and Lactobacillus acidophilus.2 As the bacteria utilize the substrate for fuel, they produce lactic acid and demineralize tooth structure. Should the environment remain favorable for their proliferation, they begin an onward march toward the dental pulp through dentin tubules. What practitioners must ascertain is what pulpal response occurs in relation to this invasion. Studies have shown that the presence or absence of bacteria is key to determining if it is possible to maintain a vital pulp.3 Thus, if bacterial incursion can be stopped or prevented, the pulp will be able to respond favorably.
Two terms, “affected” and “infected,” are key to our understanding of lesion progression. 4 Both terms are used to describe dentin and the pulp. At any given point in the development of a lesion, areas of tissue may have bacteria present (be infected). On the other hand, some areas may not have bacteria present, yet may still demonstrate physiologic changes (be affected). The areas with bacteria present are known as infected, and those that have changed but do not yet have bacteria are affected. The “million-dollar question” is this. At what point in the progression of a carious lesion does the pulp become irreversibly inflamed?
One may ask when treating deep lesions, “How can we ensure that the pulp has not been infected?” A key study by Stanley, et al, analyzed extracted teeth to determine how much remaining dentin is required in order to categorize a pulp as maintaining a healthy status.5 They found that less than 0.5 mm of remaining dentin thickness was associated with pathologic pulpal changes.6 While this thickness can only be measured histologically, it may play an important role in a practitioner’s clinical decision-making process and in reaching a proper diagnosis which will serve as the basis upon which to make a treatment recommendation.

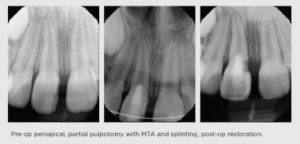
A nine-year-old female presented with luxation and a complicated enamel-dentin-cementum root fracture of her permanent maxillary right central incisor (#8). She presented two days after trauma and presented with healthy pulp tissue. Tooth #8 underwent a partial pulpotomy to a point below the fracture, SmartMTA (Sprig) and a Glass Ionomer Base (Ionostar Plus, Voco GmBh) were placed, and the tooth was restored with Filtek Supreme (3M). Her tooth was then splinted with a non-ridged splint. At subsequent recall, the tooth was restored. The tooth remains positive to vitality testing and is asymptomatic. It will be monitored per the IADT guidelines and will likely need orthodontic extrusion pending the response to pulpal therapy.
Pre-op periapical, partial pulpotomy with MTA and splinting, post-op restoration.
Diagnosis
Diagnosis is derived from the Latin word dia, meaning “through,” and the Greek verb ginoskein, meaning “to know.” To reach a diagnosis, in the words of a respected radiologist at the University of Iowa, Dr. Axel Ruprhect, “You might actually have to know something.” Currently the American Association of Endodontists recognizes the following seven pulpal diagnoses7:
Normal Pulp:
A clinical diagnostic category in which the pulp is symptom-free and normally responsive to pulp testing.
Reversible Pulpitis:
A clinical diagnosis based on subjective and objective findings indicating that the inflammation should resolve and the pulp return to normal.
Symptomatic Irreversible Pulpitis:
A clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing. Additional descriptors: lingering thermal pain, spontaneous pain, referred pain.
Asymptomatic Irreversible Pulpitis:
A clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing. Additional descriptors: no clinical symptoms but inflammation produced by caries, caries excavation, trauma.
Pulp Necrosis:
A clinical diagnostic category indicating death of the dental pulp. The pulp is usually nonresponsive to pulp testing.
Previously Treated:
A clinical diagnostic category indicating that the tooth has been endodontically treated and the canals are obturated with various filling materials other than intracanal medicaments.
Previously Initiated Therapy:
A clinical diagnostic category indicating that the tooth has been previously treated by partial endodontic therapy (e.g., pulpotomy, pulpectomy)
Vital pulp therapy focuses on the first four of these diagnoses: normal pulp, reversible pulpitis, and both asymptomatic and symptomatic irreversible pulpitis. In order to have the best chances at reaching the proper pre-treatment diagnosis, it is imperative that practitioners gather reliable evidence to reach an accurate diagnosis.
To obtain the most accurate diagnosis, clinicians must gather information from subjective and objective evaluations. The subjective evaluation should involve information that the patient provides the clinician. It includes the patient’s medical history, the chief complaint, prior history of the tooth (trauma, caries, treatment), type of pain the patient is experiencing, and what causes the pain (i.e. biting, hot, cold).
A thorough clinical exam will provide the clinician’s objective findings. The exam should include charting of restorations and decay on the tooth, visualizations of any fractures or cracks, sensibility testing such as cold and electric pulp tests, a soft tissue exam, radiographic exam, and periodontal exam.
By combining the subjective and objective findings clinicians should be able to reach a pulpal and periapical diagnosis. In the treatment of deep carious lesions and conflicting findings, caries removal may be necessary to assess restorability of the tooth and reach a pulpal diagnosis.
Challenges in Diagnosing the Pediatric Patient
While behavior may be one challenge facing a clinician when treating children, another is reaching a proper diagnosis. Children are often unreliable reporters, and parents may be poor historians. This can make gathering subjective findings difficult for providers. A diagnosis may also be compounded by the use of over-the-counter analgesics or the improper prescription of an antibiotic by another provider (i.e. a prescription when no swelling was detected).8
Sensibility testing, or pulp testing (Cold, EPT), in children also poses difficulties. The use of sensibility testing increases the reliability that a proper diagnosis is reached. Pediatric patients may not effectively communicate a positive or negative response to a test. This is compounded by the fact that the delta nerve fibers are one of the last tissues to grow into the tooth, and without these fibers, a false negative may occur.9 With immature permanent teeth, studies show that cold tests are more reliable.10 The author’s opinion is that in cases where conflicting results are reported, complete caries removal should be completed.
Indirect Pulp Therapy
Indirect pulp therapy (incomplete caries removal) is the most common choice by pediatric dentists for deep carious lesions in the cases of reversible pulpitis. This choice is based on the principal that by removing the ability of bacteria to access substrate, the carious lesion will stop growing due to the lack of fuel for proliferation. Indirect pulp therapy can be performed with a high success rate if the proper diagnosis is reached. Studies have shown that this treatment can be highly successful.
INDIRECT PULP THERAPY
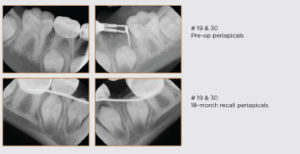
A 7-year-old male presented with multiple carious lesions on primary and permanent teeth. Of note, two lesions presented on permanent mandibular first molars with immature apices. Due to patient cooperation and the extent of dental needs, the patient was treated under general anesthesia. Teeth #19 and #30 received indirect pulp caps and full coverage restorations. Upon 18-month recall apexogenesis is evident. While currently evidence does not favor one material over another, calcium silicates such as SmartMTA deserve attention in the coming years given the sealing potential.
A wide variety of bases and liners are available on today’s market. Practitioners should give some thought as to whether a certain base or liner makes an impact on clinical outcomes. Studies have evaluated the remaining number of bacteria present in stepwise caries excavation (two visit protocol) and indicate there is no statistical difference between IRM, GI, and RMGI in the number of bacterial CFUs upon re-entry.12 This conclusion suggests there is no difference, from a bacterial standpoint, among these materials. Other literature has shown that a bioceramic will entomb bacteria in dentinal tubules. 13 While further research is needed to confirm clinical significance, it is a promising finding for practitioners utilizing these materials for indirect pulp therapy.
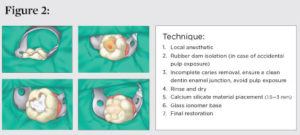
In order to be candidates for indirect or direct pulp therapy, teeth should be free of signs of necrosis and irreversible pulpitis. They should be free of spontaneous pain (or history thereof), respond to sensibility testing, be free of swelling or sinus tracts, and have normal radiographic findings. Abnormal radiographic findings include calcifications in the pulp space, apical pathosis, or a widened periodontal ligament 14 (see Figure 2).
Direct Pulp Therapy
While most endodontists practice direct caries excavation (complete caries removal, which may or may not result in a pulp exposure), it has been shown that even those who make a conscious effort to avoid pulp exposures still experience them. 15
Practitioners who plan to complete an indirect pulp therapy should be well versed in the management of a pulp exposure; in case it should occur accidentally. Current evidence also suggests that there has been an improvement in direct pulp caps due to advances made in materials led by the use of calcium silicates. Current success rates for direct pulp caps have been shown to be 80.5 percent to 96 percent. 16, 17
Historically, direct pulp caps have been carried out using calcium hydroxide (CaOH). Calcium hydroxide has a high pH which is favorable for the formation of hard tissue and is unfavorable for the proliferation of bacteria. 18 When placed in contact with the dental pulp, it forms a layer of coagulative necrosis and releases calcium ions into the pulp. Underneath the layer of necrosis, hard tissue forms. 19 The tissue that forms can be seen radiographically; however, studies show it is very porous (over 89 percent have tubular defects at two years) and that calcium hydroxide washes out over time. 20 Over the past decade, more bioceramics have entered the market. These materials are composed of tricalcium, and dicalcium silicates and have many of the same advantageous properties that are associated with calcium hydroxide. They have a high pH, are bacteriostatic, and form dentin bridges when placed in contact with the pulp. 21
This author’s opinion is that calcium hydroxide should no longer be used for direct pulp caps or pulpotomies (see Figure 3).
Pulpotomy
A pulpotomy can be performed in cases of reversible pulpitis or irreversible pulpitis. Pulpotomies are a common and familiar procedure for pediatric dentists to perform in primary teeth. The concept behind the pulpotomy is the removal of the inflamed and infected coronal pulp, while leaving healthy radicular tissue intact. This treatment is based soundly on the idea that if the pulp is free from bacteria, it can heal.
Evidence is mounting that symptomatic permanent teeth (and those vital with signs of a widened periodontal ligament) can be treated successfully with bioceramics. A retrospective study published in the Journal of Endodontics showed that teeth with clinical signs of irreversible pulpitis that were treated with a pulpotomy had a success rate of 87 percent. In comparison, teeth that had periapical lesions had a reduced success rate of 76 percent. The average recall time was 36 months. The authors concluded that clinical signs of irreversible pulpitis and the presence of periapical radiolucency should not be considered contraindications for a pulpotomy. 24
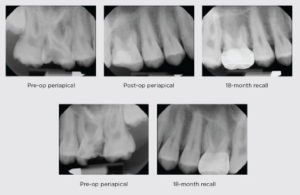
Partial pulpotomies in permanent teeth have also been shown to be highly successful in cases of irreversible pulpitis. A randomized clinical trial showed 85 percent success rate for partial pulpotomies in mature teeth at two years. The authors concluded that calcium hydroxide was not a suitable pulpotomy material 25 (see Figure 4).
DIRECT PULP THERAPY

A 12-year-old male was referred for root canal therapy of all permanent first molars. After a clinical exam, sensibility testing, and radiographs, it was determined all four molars were vital. The patient was anesthetized and rubber dam isolation was obtained. Caries excavation on the maxillary molars resulted in pulp exposures. The pulp was disinfected with sodium hypochlorite, and SmartMTA (Sprig) was placed. The teeth were restored with Ionolux (Voco GmbH). Upon recall, the tooth was restored with a stainless steel crown (3M).
PULPOTOMY


A 9-year-old female presented for a comprehensive oral evaluation. The patient was asymptomatic at the time of evaluation and had no oral complaints. Upon evaluation, a stainless-steel crown was noted on tooth #30, and a periapical radiograph was ordered, taken, and interpreted. The radiograph showed an apparent open margin on the distal, with recurrent decay, and a widened periodontal ligament. The patient was anesthetized, and rubber dam isolation was placed. The crown was removed with a high-speed handpiece. After crown removal, the patient was symptomatic even though profound anesthesia was demonstrated. A temporary restorative material was placed, and the patient was rescheduled. At a subsequent visit, the patient obtained adequate anesthesia, and the tooth was found to be vital (asymptomatic irreversible pulpitis). A pulpotomy was performed with sodium hypochlorite and SmartMTA (Sprig) as hemostasis was obtained at the canal orifice. The tooth was restored with Ionolux (Voco GmbH). At a later recall, the tooth was subsequently restored with a stainless-steel crown (3M).
CONCLUSION
When treating children with deep carious lesions in permanent teeth it is important to gather all the necessary information required to make an accurate diagnosis. Evidence suggests that many conservative options exist for treating these teeth successfully. As a practitioner who serves many patients with limited access to specialists such as endodontists, I truly believe my patients have benefited from using vital pulp therapy with calcium silicates. Perhaps we will discover that a simpler solution to these complex problems exist, if we will spend the time to make an accurate diagnosis and use the most effective materials available today.
REFERENCES
1. Koopaeei M, Inglehart M, McDonald N, Fontana M. General dentists’, pediatric dentists’, and endodontists’ diagnostic assessment and treatment strategies for deep carious lesions: A comparative analysis. J Am Dent Assoc. 2017;148(2):64–74.
2. Casamassimo P, Fields H, McTigue D, Nowak A. Pediatric Dentistry: Infancy through Adolescence. 5 ed. St Lous: Elsevier; 2013.
3. Kakehashi S, Stanley R, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surgery, Oral Medicine, Oral Pathology. 1963;20(3):340–349.
4. Mount G, Hume W. Preservation and Restoration of Tooth Structure. 2nd ed: Knowledge Books and Software; 2005.
5. Reeves R, Stanley H. The relationship of bacterial penetration and pulpal pathosis in carious teeth. Oral Surg Oral Path Oral Med. 1966:59–65.
6. De Rossi A, Bezerra Silva L, Gaton-Hernandez P, et al. Comparison of Pulpal Responses to Pulpotomy and Pulp Capping with Biodentine and Mineral Trioxide Aggregate in Dogs. J Endod. 2014;40:1362–1369.
7. American Association of Endodontics. AAE Consensus Conference Recommendation Diagnostic Terminology. J Endod. 2009;35:163– 164.
8. Read J, McClanahan S, Khan A, Lunos S, Bowles W. Effect of Ibuprofen on masking endodontic diagnosis. J Endod. 2014;40(8): 1058–62.
9. Johnsen D. Innervation of Teeth: Qualitative, Quantitative, and Developmental Assessment. J Dent Res. Apr 1985;64:555–63.
10. Levin LG. Pulp and Periradicular Testing. Pediatr Dent. 2013;32:125–128.
11. Maltz M, de Oliveira E, Fontanella V, Bianchi R. A clinical, microbiologic, and radiographic study of deep caries lesions after incomplete caries removal. Quintessence Int. 2002;33(2):151–159.
12. Duque C, Negrini T, Sanco N, Spolidorio D, Alberto de Souza Costa C, Hebling J. Clinical and microbiologic performance of resin-modified glass-ionomer liners after incomplete dentine caries removal. Clin Oral Invest. 2009;13:465–471.
13. Yoo J, Chang S, Oh S, et al. Bacterial entombment by intratubular mineralization following orthograde mineral trioxide aggregate obturation: a scanning electron microscopy study. Int Jour Oral Sci. 2014(6):227–32.
14. Orhan A, Oz F, Orhan K. Pulp Exposure Occurance and Outcomes after 1- or 2-visit Indirect Pulp Therapy Vs. Complete Caries Removal in Primary and Permanent Molars. Pediatr Dent. July/Aug 2010;32(4):347–355.
15. Leksell E, Ridell K, Cvek M, Mejare I. Pulp exposure after stepwise versus direct complete excavation of deep carious lesions in young posterior permanent teeth. Endod Dent Traumatol. 1996;12:192–196.
16. Miles J, Gluskin A, Chambers D, Peters O. Pulp capping with mineral trioxide aggregate (MTA): a retrospective analysis of carious pulp exposures treated by undergraduate dental students. Oper Dent. 2010;35(1):20–28.
17. Bogen G, Kim J, Bakland L. Direct Pulp Capping with Mineral Trioxide Aggregate: an Observational Study. J Am Dent Assoc. 2008;139(3):305–315.
18. Stanley H. Pulp capping: Conserving the dental pulp—Can it be done? Is it worth it? Oral Surg Oral Med Oral Pathol. 1989;68:628–639.
19. Cox C, Keall C, Keall H, Ostro E, Bergenholtz G. Biocompatibility of surface-sealed dental materials against exposed pulps. J Prosth Dent. 1987;57(1):1–8.
20. Cox C, Subay R, Ostro E, Suzuki S, Suzuki S. Tunnel defects in dentinal bridges: their formation following direct pulp-capping. Oper Dent. 1996;21:4–11.
21. Sakar N, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physiochemical Basis of the Biologic Properties of Mineral Trioxide Aggregate. J Endod. 2005;31(2):97–100.
22. Camilleri J. Staining Potential of Neo MTA Plus, MTA, Plus, and Biodentine Used for Pulpotomy Procedures. J Endod. 2015;41(7): 1139–45.
23. Bogen G. Protocol: Direct Pulp Capping Using MTA Two-Visit Technique. Nd.
24. Linsuwanont P, Wimonsutthikul K, Pothimoke U, Santiwong B. Treatment Outcomes of Mineral Trioxide Aggregate Pulpotomy in Vital Permanent Teeth with Carious Pulp Exposure: The Retrospective Study. J Endod. Feb 2017;43(2):225–30.
25. Taha N, Khazali M. Partial Pulpotomy in Mature Permanent Teeth with Clinical Signs Indicative of Irreversible Pulpitis: A Randomized Clinical Trial. J Endod. Sep 2017;43(9):1417–21.
26. Schwendicke F, Stolpe M. Direct Pulp Capping after a Carious Exposure Versus Root Canal Treatment: A Cost-effectiveness Analysis. J Endod. November 2014;40(11):1764–1770.
27. Cobourne M, Williams A, Harrison M. A Guideline for the Extraction of Permanent Molars in Children. London: Royal College of Surgeons; 2014.
28. Mente J, Hufnagel S, Leo M. Treatment Out Come of Mineral Trioxide Aggregate or Calcium Hydroxide Direct Pulp Capping: Long-term Results. J Endod. 2014;40(11):1746–51.
Originally published in Shift Magazine Spring 2019


